
ADHD & Sleep
The links between ADHD and sleep issues are still unclear, as is the cause of ADHD in general. Both the symptoms of ADHD and some of its medications can affect sleeping patterns. Also, “sleep deprivation…can worsen ADHD symptoms.” Nearly 50% of kids with ADHD suffer from some sort of sleep problem and nearly 75% of adults with ADHD reported suffering from insomnia.
Common Sleep Problems Associated with ADHD:
- Anxiety or resistance about bedtime (in children)
- Difficulty falling asleep at night
- Difficulty waking up in the morning
- Sleep-disordered breathing and sleep apnea
- Interrupted sleep (waking up during the night)
- Excessive daytime sleepiness
- Restless legs syndrome (RLS)
- Periodic limb movement disorder (PLMD)
- Delayed sleep-phase disorder
- Higher rates of nightmares
- More likely than average to experience parasomnias like sleepwalking
Treatments for these ADHD-related sleep issues include cognitive behavioral therapy (CBT) and medication management. Contact Dr. Bharagava’s office to see if these treatments may help you or your child’s ADHD symptoms.
Source: “ADHD and Sleep” by Tuck.com
Gabby Lundy, Exult Healthcare

What Treatments Do Psychiatrists Use?
Treatment Types:
-
Psychotherapy
-
Medications
-
Psychosocial Interventions
-
TMS
-
Other Physical Treatments (Less Common):
- ETC, DBS, & VNS
Psychotherapy is often the first step with patients. From there, a psych eval will be done and it will be determined if the patient would benefit from a medication plan.
Class of Medications:
- Antidepressants – used to treat depression, panic disorder, PTSD, anxiety, obsessive-compulsive disorder, borderline personality disorder and eating disorders
- Antipsychotic medications – used to treat psychotic symptoms (delusions and hallucinations), schizophrenia, bipolar disorder
- Sedatives and anxiolytics – used to treat anxiety and insomnia
- Hypnotics – used to induce and maintain sleep
- Mood stabilizers – used to treat bipolar disorder
- Stimulants – used to treat ADHD
These medications can “help correct imbalances in brain chemistry that are thought to be involved in some mental disorders.” Psychiatrists are one of the few mental health providers that can prescribe medication and are usually a necessary piece of long-term medication management for mental health issues.
Source: “What is Psychiatry?” American Psychiatric Association
Gabby Lundy, Exult Healthcare

Mental Health & Chronic Illness: Selena Gomez
Last Wednesday, pop singer and television producer, Selena Gomez was admitted to a psychiatric hospital. She is told to have suffered a panic attack after a recent health setback related to her two recent hospitalizations for “low blood cell count” post-kidney transplant. Gomez has Lupus and underwent a kidney transplant in September of 2017 because of Lupus-related complications.
Selena Gomez has been open about her struggles with Lupus–a chronic illness that causes –and with mental health since 2015. Early in 2018, Gomez received outpatient psychiatric treatment to address anxiety. However, Gomez is not the only person whose mental health has suffered as a result of dealing with a chronic illness.
Chronic Illness and Depression
Chronic illnesses of all kinds can cause or worsen depression in the following ways:
- Increased feelings of isolation
- Taking off more time from work, school & social events for treatment and self-care
- Feeling like no one understands your condition
- Increased fatigue in some chronic illnesses may make depression-related fatigue worse
- Inflammation symptoms (in some chronic illnesses such as Lupus) which have some evidence pointing to causing or worsening depression
- Enhanced life, work, financial, and relationship stressors as a result of the chronic illness
Taking control of your mental health can be one piece of dealing with a chronic illness and your overall health. Doctor Heals Mind has a variety of treatments available for depression and other mental health issues. Please check out our depression treatment page to find a solution that best fits your needs.
By: Gabby Lundy, Exult Healthcare

Who Can Help Treat My Depression?
Mental health treatment can be found from a variety of professionals, especially for depression. Knowing your own symptoms and needs can help you determine what type of care provider is needed to best treat your depression. You may even see more than one of these professionals at a time to get the best care possible. Let’s break down some differences between these mental health care professionals.
Primary Care Doctors
Your general doctor may be the first person you see to access care. They can:
- Recommend a behavioral health provider such as a therapist, counselor, psychiatrist, etc.
- Prescribe and monitor medication
- Monitor your progress and follow up over time
Psychiatrists
Psychiatrists have medical degrees (MD) and specific training in mental health conditions. They can:
- Assess your symptoms to make an informed diagnosis
- Assess the need for medication
- Prescribe and monitor medication
- Provide psychotherapy
Licensed Counselors, Therapist, and Social Workers
All three of these providers have a master’s degree (MS), a doctorate (Ph.D.), or another type of graduate-level certification. They have completed an internship and one (or more) years of supervised practice. They can:
- Assess your symptoms to make an informed diagnosis
- Provide talk therapy (also known as counseling)
- Offer specialized counseling, such as family or marriage therapy
Psychologists
Psychologists have a master’s degree (MS) or a doctorate (Ph.D./PsyD) in psychology. They are not medical doctors nor can they prescribe medication (in most cases). However, they can:
- Assess your symptoms to make an informed diagnosis
- Provide talk therapy (also known as counseling)
- Conduct psychological testing
- Refer you to a psychiatrist for medication
Psychiatric Nurse Practitioners
Psychiatric nurses are register nurses (RN) that also have graduate-level education in mental health. They can:
- Assess psychiatric conditions
- Prescribe and monitor medication
- Follow up with medication management and coordination of care
If you feel like medication may be part of your mental health treatment, Dr. Bhargava, a board-certified psychiatrist, may be able to help. Visit our Depression Treatment page for more information.
If you are more interested in talk therapy, Exult Healthcare has licensed therapists and counselors that have a variety of specialties. They also offer transcranial magnetic stimulation (TMS) treatment if therapy and medications are not working for you.
Source: https://www.aetna.com/individuals-families/mental-emotional-health/depression-care-providers.html
Gabby Lundy, Exult Healthcare

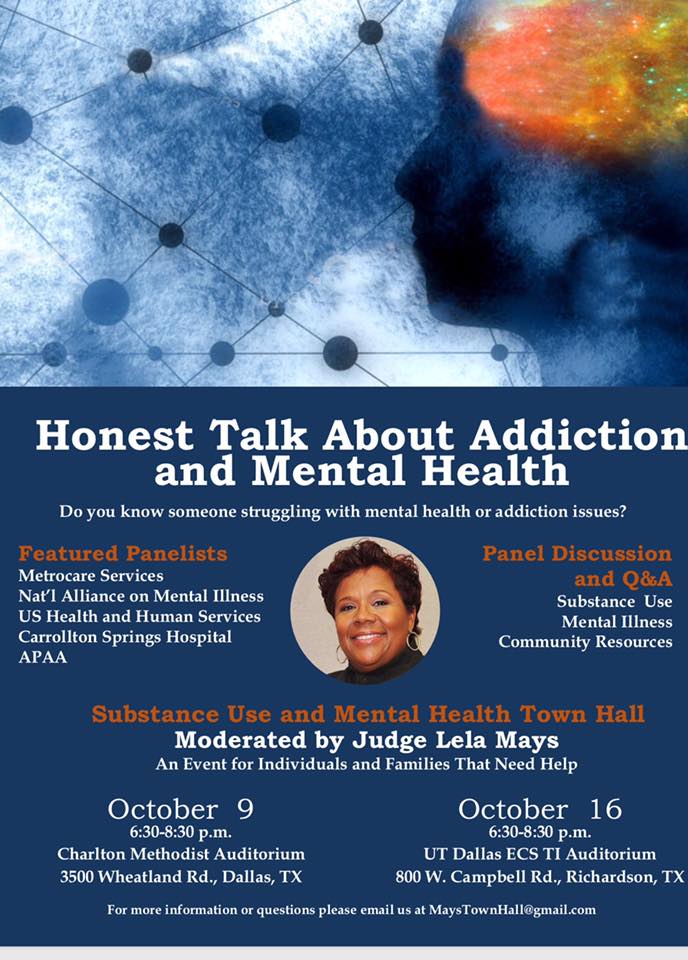
Dr. B Speaks on “Honest Talk About Mental Health and Addiction” Panel

Last night, Dr. Bhargava spoke on a local panel discussing substance abuse, mental health, and local resources for support. The town hall event—moderated by Judge Lela Mays—featured panelists from a variety of government and healthcare services related to mental health and addiction to answer questions about community resources and funding issues.
Missed the discussion? Dr. B will be participating in the next panel which will be held on October 16th from 6:30-8:30 p.m. at UT Dallas ECS TI Auditorium. (See flyer for more details.)
By: Gabby Lundy, Exult Healthcare
College Depression
“Going to college is an exciting time in the lives of young people, but for some students depression gets in the way. Whether it’s their first brush with the disorder or not, college can act as a catalyst for the onset of depression in many young people, and, on their own for the first time, the timing couldn’t be worse” – childmind.org
Depression in college students is a topic that is not often talked about but is common for first semester college students. Most of the time, first semester students have a hard time adjusting to a new environment; picking up a heavy work load, being away from home, and have to make new friends. Parents can often worry and try to get involved, but that’s not always easy when a child is potentially living three to four hours away from home. If you have a student that is distancing themselves from the outside world, letting go of their hobbies and ambitions, and acting out of character for more than two weeks it is possible that your college student could be facing depression.

Depression is not always an easy topic to discuss, and most people only think an individual is depressed when they are sad. That is not the case, depression comes in many forms. For some students, it could be that he or she is more irritable, lashes out, and pushes away their support systems (friends, family, significant others). Other students could be indulging in binge drinking or substance abuse to try to “forget about their problems” or “make their problems go away”. It is important to notice the signs and act quickly. Encourage your student to seek on campus help or seek help in their area.
If you are worried about your college student and feel that they are facing depression and do not want to acknowledge it themselves, Exult Healthcare has services that can benefit you. Depression is usually treated with medications, psychotherapy, or a combination of the two. If these treatments do not reduce symptoms, transcranial magnetic stimulation (TMS) and other brain stimulation therapies
may be options to explore. However, each case of depression is unique and is treated accordingly. There is never a “one-size-fits-all” for treatments here. Please check out our treatments tab and find out more about how Exult Healthcare can benefit you today.
Written By: Lauren Thompson, Exult Healthcare
BINGE EATING
Binge eating disorder develops based on a mixture of genetic, environmental and social constructs. The focus on this blog is the social/ family aspect of eating patterns.
Food is such a major component of cultural, social and family dynamics. It is used as part of celebrations, for religious ritualization, cultural events and a learned self-soothing habit. We have cake for birthday parties, a cultural dish to help when you are sick (like chicken soup), and a special treat when you are sad (warm cookies) or a special dinner on major occasions. Having food for every occasion can lend to the use of food as a negative coping skill because it has become a learned behavior. Binge eating / obesity will run in families due to the way food is used to deal with feeling or emotions. Memories are strongly tied to our senses: taste reminds use of a positive experience, the smell of food may remind us of a family member that cooked, and touch could be helping cook a special meal and the sound of a specific food cooking to bring back a special memory.
“From infancy, we establish a connection with our caregivers based on how our most instinctual needs are met. “ (Karges, 2018) One of our most instinctual needs is food and it is a major part of the bonding moments with a mother. According to Hamberg, The sharing of food can increases closeness to others like our parents making our favorite dessert when we are upset or sharing food at times of crisis. The use of food can become a supportive behavior and if no other self-soothing behavior is taught then food become the primary means to sooth self and others. The use of food in as a coping and self-soothing tool within the family can lead to binge eating disorders among members. According to Karges, some ways self-soothing through food is taught is by giving a food as a reward, a bribery to behave a certain way or used to comfort a child in destress. It is like replacing their favorite blanket or toy with a cookie every time they get upset.
There is also a genetic connection with binge eating and comorbid disorders like depression so families have learned to cope with the depression by using food. In the study, Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity, There is a correlation between parental mental illness and binge eating disorder and children developing the same patterns of behavior and diagnosis. If the behavior continues then it will be passed down multi-generationally.
The best way to assist in treating or preventing binge eating disorder is through the family system by changing eating patterns and the use of food in emotional regulation. In order for recovery to become effective the family needs to be involved in treatment to help reduce familial patterns in future generations and to support positive change.
References
Braden AL, Madowitz J, Matheson BE, Bergmann K, Crow SJ, Boutelle KN. Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity. Child Obes. 2015;11:1659. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4382825/
Hamburg, M. E., Finkenauer, C., & Schuengel, C. (2014). Food for love: The role of food offering in empathic emotion regulation. Frontiers in Psychology, 5. doi:10.3389/fpsyg.2014.00032 https://www.frontiersin.org/articles/10.3389/fpsyg.2014.00032/full
Karges, K. (2018). Binge Eating Disorder and Family Patterns of Self-Soothing. Eating Disorder Hope. Retrieved from https://www.eatingdisorderhope.com/information/binge-eating-disorder/binge-eating-disorder-and-family-patterns-of-self-soothing.
Written By: Karen Limme LPC Intern, Exult Healthcare
Chester Bennington: One Year
It has been a year since Chester Bennington, front-man of rock group Linkin Park, died by suicide. It was a shock that was seen from both rock music lovers to the general public.
The death was not the first and would not be the last in a string from 2017 to 2018. But it does emphasis the power of music therapy for many and an unity that followed his death.
Bennington had opened up about how music positively contributed to his mental health recovery process. In an interview Bennington said, “ It’s cool to be a part of recovery. This is just who I am, this is what I write about, what I do, and most my work has been a reflection of what I’ve been going through in one way or another.”
His fight with depression and mental health was an informative resource for his fans. His legacy can be seen in the tidal wave of support and initiative that came from his memory.
Talinda Bennington, Bennington’s wife, began a partnership with “Give an Hour” and “Change Direction”. Both programs main focus is to assist and raise awareness of mental health.
Today, July 20th, marks the anniversary of his death by suicide. His life is honored by the amount of awareness and support the mental health community has received.
His fellow bandmates Mike Shinoda, Joe Han, Dave Farrell, Rob Bourdon, and Brad Delson wrote, “To our brother Chester, it has been a year since your passing — a surreal rotation of grief, heartbreak, refusal, and recognition. And yet it (still) feels like you are close by, surrounding us with your memory and your light.”
#MakeChesterProud
tr(EAT)ing Your Issues
Many people suffer from both physical and mental issues ranging from chronic pain to depression and addiction, and many of them don’t want to rely on prescription medications of expensive professional therapies to help them manage. While there is a place for that in some cases, one of the best and most effective things you can do right now to help yourself is change your diet for the better.
Obesity is the leading cause of dozens of ailments
The benefits of losing weight stretch far beyond looking good in a bikini. Being obese is the leading cause of a wide range of health problems, and it’s one of the health conditions that’s well within your control. With a healthy diet, you can eliminate obesity and move toward a healthy weight.
Here’s a short list of conditions that obesity plays a role in: high blood pressure, high LDL cholesterol, low HDL cholesterol, or high levels of triglycerides, type 2 diabetes, coronary heart disease, stroke, and some cancers (endometrial, breast, colon, kidney, gallbladder, and liver).
Obesity also plays a part in mental health issues like depression and anxiety. It puts a strain on muscles and joints, leading to chronic pain.
The point is, reducing your weight through a dietary change is the best thing you can do to address whatever ails you.
What you eat directly influences your mood
For those suffering from mental illness, eating the right food and avoiding the wrong food can be one of your best lines of defense. What you put in your gut is what powers your brain. If you’re giving your “engine” low-quality fuel, you’re going to see low-quality results.
One thing you can do immediately is ween yourself off refined sugars – including soft drinks, sweet tea, sugary cereals, and desserts. “Multiple studies have found a correlation between a diet high in refined sugars and impaired brain function — and even a worsening of symptoms of mood disorders, such as depression,”says Harvard Health. .
You can eat certain foods that contain vitamins and nutrients that have been shown to boost mental health. “Evidence suggests that certain nutrients in food may support emotional well-being. These include nutrients such as omega-3 fatty acids, folic acid, vitamin D, and vitamin B-12,”notes FamilyDoctor.org.
Fatty fish like salmon and mackerel, nuts, leafy greens, and low-fat dairy all fit the bill.
Trading healthy habits for unhealthy ones
Healthy eating is about discipline and control. Learning how to limit your food intake, avoid unhealthy (but tempting) foods, and stick to a plan all teach your brain that you have the power of self-control.
Turning to “comfort eating” to help cope with problems mimics the behavior of drug and alcohol addiction and can lead you down a bad path.
“Another problem with comfort eating is that it is just another way to avoid dealing with problems. It is similar to alcohol and drug addiction as it actually increases the problems that people will have to deal with,” says AlcoholRehab.com.
Healthy eating also reduces spikes in blood sugar, which has been shown to be a problem for those in recovery.
Before you invest in expensive treatments or turn to prescription medication to deal with your physical or mental ailments, you should reassess your diet and see if you can make some changes for the better. Start small. It may sound cliche, but Rome really wasn’t built in a day. A healthy diet is a lifestyle choice, not a weekly fad. The more you work healthy eating into your daily routine and make it a part of your life, the better you’ll be able to stick to it as the weeks, months, and years go by.
By: Guest Writer, Eric Johnson from Us Health Corps
The views of this author are not that of Exult Healthcare, and therefore, are the individual’s own views.
Minding Your Upkeep
“Mindfulness is the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally, to things as they are.”
-Williams, Tisdale, Segal and Kabat-Zinn
Mindfulness
Moment-to-moment awareness 
Being in the present
Cultivate a new kind of control and wisdom
Inner relaxation
Knowledge of self
Acceptance
Directing attention
(Kabat-Zinn, 1990) & (Baer, 2006)
Strategies for Developing with Mindfulness:
Be mindful of one thing at a time- internal or external not both.
Be nonjudgmental- describe what you are observing without making a judgment. Enjoy the moment.
Patience
Beginner mind- look at thing through new eyes
Slow down
Stop-be still and silent in meditation
Trust- develop a trust in yourself
Non-striving- no goal
Observe-participant observer by engaging with the experience
Be mindful of the moment- observe the present without thinking of the past or future.
Focus on your senses- use all your senses in the moment to truly appreciate the event or observation
Return- when you wonder off return back to your focus
(Kabat-Zinn, 1990)
Major Concepts in Mindfulness:
Present
The only time we have to:
Know
Perceive
Learn
Act
Change
Heal
(Kabat-Zinn, 1990)
Being
Lack of a goal
“Letting go of wanting something else to happen.” (Kabat-Zinn, 1994, p. 15)
Being more aware of ourselves
Present- moment-to-moment experience
Accepting things how they are
Allowing things to be as they are
Thoughts are passing events in the mind
(Segal, Williams & Teasdale, 2013)
Breath
Focus on the breath without controlling the breath.
Watch your stomach move up and down or place your hand on it as it moves
Attention to the feeling on your breath entering and exiting
The focus helps avoid your mind wondering
Calms the anxious mind
Takes us back to now- breath is only now
(Kabat-Zinn, 2012)
Driven and Doing
Don’t let go of a goal
Consumed with solving the problem
Difference in how things are and how you want them to be
Ruminating- focus on past and future
Affects view of self
Ignore the present
Driven by expectations
Have our own way
(Segal, Williams & Teasdale, 2013)
Written by: Dr. Cynthia D’Sauza, Clinical Director
References
Baer, R. A.(2006). Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications. San Diego: Elsevier Academic Press.
Kabat-Zinn, J. (2012). Mindfulness for beginners. Boulder: Sounds True.
Kabat-Zinn, J. (2007). The MBCT program. Retrieved from http://mbct.com/Classes_Main.htm
Kabat-Zinn, J. (1994). Wherever you go, there you are. New York: MFJ Books.
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness (15th anniversary ed.): New York: Delta Trade Paperback/Bantam Dell.
Segal, Z., Williams, M., & Teasdale, J. (2013) Mindfulness-based cognitive therapy for depression. New York: Guilford Press.
Williams, M., Teasdale, J., Segal, Z., & Kabat-Zinn, J. (2007). The mindful way through depression: Freeing yourself from chronic unhappiness. New York: Guilford Press.

