
NeuroStar TMS
About NeuroStar TMS
NeuroStar Advanced Therapy (TMS) for depression has the largest clinical data set of any TMS treatment. Clinical studies with over 900 people have shown that NeuroStar may help achieve remission for people living with depression.
For many people, depression symptoms significantly improved or went away after 4 to 6 weeks of treatment with NeuroStar Advanced Therapy.
In a NIMH-funded, independent, randomized, controlled trial, people treated with TMS NeuroStar Advanced Therapy were four times more likely to achieve remission compared to patients receiving the placebo treatment!
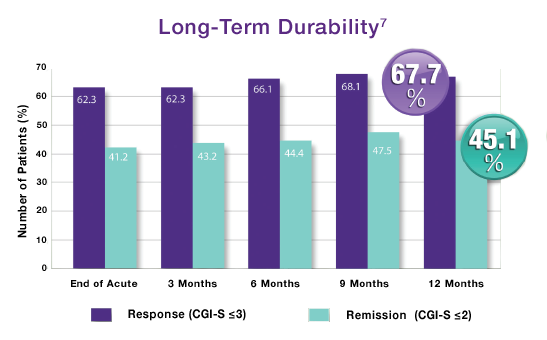
Only NeuroStar Advanced Therapy (TMS) has durability over 12 months.
Source: NeuroStar TMS Therapy Clinical Results
Gabby Lundy, Exult Healthcare

What Treatments Do Psychiatrists Use?
Treatment Types:
-
Psychotherapy
-
Medications
-
Psychosocial Interventions
-
TMS
-
Other Physical Treatments (Less Common):
- ETC, DBS, & VNS
Psychotherapy is often the first step with patients. From there, a psych eval will be done and it will be determined if the patient would benefit from a medication plan.
Class of Medications:
- Antidepressants – used to treat depression, panic disorder, PTSD, anxiety, obsessive-compulsive disorder, borderline personality disorder and eating disorders
- Antipsychotic medications – used to treat psychotic symptoms (delusions and hallucinations), schizophrenia, bipolar disorder
- Sedatives and anxiolytics – used to treat anxiety and insomnia
- Hypnotics – used to induce and maintain sleep
- Mood stabilizers – used to treat bipolar disorder
- Stimulants – used to treat ADHD
These medications can “help correct imbalances in brain chemistry that are thought to be involved in some mental disorders.” Psychiatrists are one of the few mental health providers that can prescribe medication and are usually a necessary piece of long-term medication management for mental health issues.
Source: “What is Psychiatry?” American Psychiatric Association
Gabby Lundy, Exult Healthcare
College Depression
“Going to college is an exciting time in the lives of young people, but for some students depression gets in the way. Whether it’s their first brush with the disorder or not, college can act as a catalyst for the onset of depression in many young people, and, on their own for the first time, the timing couldn’t be worse” – childmind.org
Depression in college students is a topic that is not often talked about but is common for first semester college students. Most of the time, first semester students have a hard time adjusting to a new environment; picking up a heavy work load, being away from home, and have to make new friends. Parents can often worry and try to get involved, but that’s not always easy when a child is potentially living three to four hours away from home. If you have a student that is distancing themselves from the outside world, letting go of their hobbies and ambitions, and acting out of character for more than two weeks it is possible that your college student could be facing depression.

Depression is not always an easy topic to discuss, and most people only think an individual is depressed when they are sad. That is not the case, depression comes in many forms. For some students, it could be that he or she is more irritable, lashes out, and pushes away their support systems (friends, family, significant others). Other students could be indulging in binge drinking or substance abuse to try to “forget about their problems” or “make their problems go away”. It is important to notice the signs and act quickly. Encourage your student to seek on campus help or seek help in their area.
If you are worried about your college student and feel that they are facing depression and do not want to acknowledge it themselves, Exult Healthcare has services that can benefit you. Depression is usually treated with medications, psychotherapy, or a combination of the two. If these treatments do not reduce symptoms, transcranial magnetic stimulation (TMS) and other brain stimulation therapies
may be options to explore. However, each case of depression is unique and is treated accordingly. There is never a “one-size-fits-all” for treatments here. Please check out our treatments tab and find out more about how Exult Healthcare can benefit you today.
Written By: Lauren Thompson, Exult Healthcare
BINGE EATING
Binge eating disorder develops based on a mixture of genetic, environmental and social constructs. The focus on this blog is the social/ family aspect of eating patterns.
Food is such a major component of cultural, social and family dynamics. It is used as part of celebrations, for religious ritualization, cultural events and a learned self-soothing habit. We have cake for birthday parties, a cultural dish to help when you are sick (like chicken soup), and a special treat when you are sad (warm cookies) or a special dinner on major occasions. Having food for every occasion can lend to the use of food as a negative coping skill because it has become a learned behavior. Binge eating / obesity will run in families due to the way food is used to deal with feeling or emotions. Memories are strongly tied to our senses: taste reminds use of a positive experience, the smell of food may remind us of a family member that cooked, and touch could be helping cook a special meal and the sound of a specific food cooking to bring back a special memory.
“From infancy, we establish a connection with our caregivers based on how our most instinctual needs are met. “ (Karges, 2018) One of our most instinctual needs is food and it is a major part of the bonding moments with a mother. According to Hamberg, The sharing of food can increases closeness to others like our parents making our favorite dessert when we are upset or sharing food at times of crisis. The use of food can become a supportive behavior and if no other self-soothing behavior is taught then food become the primary means to sooth self and others. The use of food in as a coping and self-soothing tool within the family can lead to binge eating disorders among members. According to Karges, some ways self-soothing through food is taught is by giving a food as a reward, a bribery to behave a certain way or used to comfort a child in destress. It is like replacing their favorite blanket or toy with a cookie every time they get upset.
There is also a genetic connection with binge eating and comorbid disorders like depression so families have learned to cope with the depression by using food. In the study, Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity, There is a correlation between parental mental illness and binge eating disorder and children developing the same patterns of behavior and diagnosis. If the behavior continues then it will be passed down multi-generationally.
The best way to assist in treating or preventing binge eating disorder is through the family system by changing eating patterns and the use of food in emotional regulation. In order for recovery to become effective the family needs to be involved in treatment to help reduce familial patterns in future generations and to support positive change.
References
Braden AL, Madowitz J, Matheson BE, Bergmann K, Crow SJ, Boutelle KN. Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity. Child Obes. 2015;11:1659. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4382825/
Hamburg, M. E., Finkenauer, C., & Schuengel, C. (2014). Food for love: The role of food offering in empathic emotion regulation. Frontiers in Psychology, 5. doi:10.3389/fpsyg.2014.00032 https://www.frontiersin.org/articles/10.3389/fpsyg.2014.00032/full
Karges, K. (2018). Binge Eating Disorder and Family Patterns of Self-Soothing. Eating Disorder Hope. Retrieved from https://www.eatingdisorderhope.com/information/binge-eating-disorder/binge-eating-disorder-and-family-patterns-of-self-soothing.
Written By: Karen Limme LPC Intern, Exult Healthcare

