
NeuroStar TMS
About NeuroStar TMS
NeuroStar Advanced Therapy (TMS) for depression has the largest clinical data set of any TMS treatment. Clinical studies with over 900 people have shown that NeuroStar may help achieve remission for people living with depression.
For many people, depression symptoms significantly improved or went away after 4 to 6 weeks of treatment with NeuroStar Advanced Therapy.
In a NIMH-funded, independent, randomized, controlled trial, people treated with TMS NeuroStar Advanced Therapy were four times more likely to achieve remission compared to patients receiving the placebo treatment!
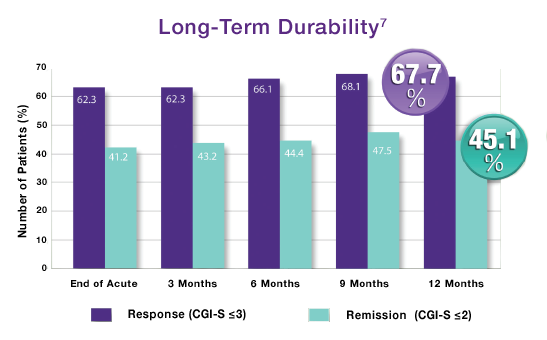
Only NeuroStar Advanced Therapy (TMS) has durability over 12 months.
Source: NeuroStar TMS Therapy Clinical Results
Gabby Lundy, Exult Healthcare

ADHD & Sleep
The links between ADHD and sleep issues are still unclear, as is the cause of ADHD in general. Both the symptoms of ADHD and some of its medications can affect sleeping patterns. Also, “sleep deprivation…can worsen ADHD symptoms.” Nearly 50% of kids with ADHD suffer from some sort of sleep problem and nearly 75% of adults with ADHD reported suffering from insomnia.
Common Sleep Problems Associated with ADHD:
- Anxiety or resistance about bedtime (in children)
- Difficulty falling asleep at night
- Difficulty waking up in the morning
- Sleep-disordered breathing and sleep apnea
- Interrupted sleep (waking up during the night)
- Excessive daytime sleepiness
- Restless legs syndrome (RLS)
- Periodic limb movement disorder (PLMD)
- Delayed sleep-phase disorder
- Higher rates of nightmares
- More likely than average to experience parasomnias like sleepwalking
Treatments for these ADHD-related sleep issues include cognitive behavioral therapy (CBT) and medication management. Contact Dr. Bharagava’s office to see if these treatments may help you or your child’s ADHD symptoms.
Source: “ADHD and Sleep” by Tuck.com
Gabby Lundy, Exult Healthcare

What Treatments Do Psychiatrists Use?
Treatment Types:
-
Psychotherapy
-
Medications
-
Psychosocial Interventions
-
TMS
-
Other Physical Treatments (Less Common):
- ETC, DBS, & VNS
Psychotherapy is often the first step with patients. From there, a psych eval will be done and it will be determined if the patient would benefit from a medication plan.
Class of Medications:
- Antidepressants – used to treat depression, panic disorder, PTSD, anxiety, obsessive-compulsive disorder, borderline personality disorder and eating disorders
- Antipsychotic medications – used to treat psychotic symptoms (delusions and hallucinations), schizophrenia, bipolar disorder
- Sedatives and anxiolytics – used to treat anxiety and insomnia
- Hypnotics – used to induce and maintain sleep
- Mood stabilizers – used to treat bipolar disorder
- Stimulants – used to treat ADHD
These medications can “help correct imbalances in brain chemistry that are thought to be involved in some mental disorders.” Psychiatrists are one of the few mental health providers that can prescribe medication and are usually a necessary piece of long-term medication management for mental health issues.
Source: “What is Psychiatry?” American Psychiatric Association
Gabby Lundy, Exult Healthcare

Mental Health & Chronic Illness: Selena Gomez
Last Wednesday, pop singer and television producer, Selena Gomez was admitted to a psychiatric hospital. She is told to have suffered a panic attack after a recent health setback related to her two recent hospitalizations for “low blood cell count” post-kidney transplant. Gomez has Lupus and underwent a kidney transplant in September of 2017 because of Lupus-related complications.
Selena Gomez has been open about her struggles with Lupus–a chronic illness that causes –and with mental health since 2015. Early in 2018, Gomez received outpatient psychiatric treatment to address anxiety. However, Gomez is not the only person whose mental health has suffered as a result of dealing with a chronic illness.
Chronic Illness and Depression
Chronic illnesses of all kinds can cause or worsen depression in the following ways:
- Increased feelings of isolation
- Taking off more time from work, school & social events for treatment and self-care
- Feeling like no one understands your condition
- Increased fatigue in some chronic illnesses may make depression-related fatigue worse
- Inflammation symptoms (in some chronic illnesses such as Lupus) which have some evidence pointing to causing or worsening depression
- Enhanced life, work, financial, and relationship stressors as a result of the chronic illness
Taking control of your mental health can be one piece of dealing with a chronic illness and your overall health. Doctor Heals Mind has a variety of treatments available for depression and other mental health issues. Please check out our depression treatment page to find a solution that best fits your needs.
By: Gabby Lundy, Exult Healthcare

Who Can Help Treat My Depression?
Mental health treatment can be found from a variety of professionals, especially for depression. Knowing your own symptoms and needs can help you determine what type of care provider is needed to best treat your depression. You may even see more than one of these professionals at a time to get the best care possible. Let’s break down some differences between these mental health care professionals.
Primary Care Doctors
Your general doctor may be the first person you see to access care. They can:
- Recommend a behavioral health provider such as a therapist, counselor, psychiatrist, etc.
- Prescribe and monitor medication
- Monitor your progress and follow up over time
Psychiatrists
Psychiatrists have medical degrees (MD) and specific training in mental health conditions. They can:
- Assess your symptoms to make an informed diagnosis
- Assess the need for medication
- Prescribe and monitor medication
- Provide psychotherapy
Licensed Counselors, Therapist, and Social Workers
All three of these providers have a master’s degree (MS), a doctorate (Ph.D.), or another type of graduate-level certification. They have completed an internship and one (or more) years of supervised practice. They can:
- Assess your symptoms to make an informed diagnosis
- Provide talk therapy (also known as counseling)
- Offer specialized counseling, such as family or marriage therapy
Psychologists
Psychologists have a master’s degree (MS) or a doctorate (Ph.D./PsyD) in psychology. They are not medical doctors nor can they prescribe medication (in most cases). However, they can:
- Assess your symptoms to make an informed diagnosis
- Provide talk therapy (also known as counseling)
- Conduct psychological testing
- Refer you to a psychiatrist for medication
Psychiatric Nurse Practitioners
Psychiatric nurses are register nurses (RN) that also have graduate-level education in mental health. They can:
- Assess psychiatric conditions
- Prescribe and monitor medication
- Follow up with medication management and coordination of care
If you feel like medication may be part of your mental health treatment, Dr. Bhargava, a board-certified psychiatrist, may be able to help. Visit our Depression Treatment page for more information.
If you are more interested in talk therapy, Exult Healthcare has licensed therapists and counselors that have a variety of specialties. They also offer transcranial magnetic stimulation (TMS) treatment if therapy and medications are not working for you.
Source: https://www.aetna.com/individuals-families/mental-emotional-health/depression-care-providers.html
Gabby Lundy, Exult Healthcare

Suboxone Onsite
Suboxone (Buprenorphine/Naloxone) Onsite
Our facility provides Medicated-Assisted Treatment (MAT) for Suboxone (Buprenorphine/Naloxone).
Medicated-Assisted Treatment (MAT) is the use of FDA- approved medications, in combination with counseling and behavioral therapies, to provide a “whole-patient” approach to the treatment of substance use disorders.
We follow an integrated approach that includes med management, counseling and behavioral therapies.
Our physicians have taken the proper training and are approved to safely administer Suboxone to treat opiate addiction. We have trained counselors and therapists to offer behavioral therapies.
Medications Used in MAT
FDA has approved several different medications to treat opioid addiction and alcohol dependence.
A common misconception associated with MAT is that it substitutes one drug for another. Instead, these medications relieve the withdrawal symptoms and psychological cravings that cause chemical imbalances in the body. MAT programs provide a safe and controlled level of medication to overcome the use of an abused opioid. And research has shown that when provided at the proper dose, medications used in MAT have no adverse effects on a person’s intelligence, mental capability, physical functioning, or employability.
Medications used in MAT for opioid treatment can only be dispensed through a SAMHSA-certified OTP. Some of the medications used in MAT are controlled substances due to their potential for misuse. Drugs, substances, and certain chemicals used to make drugs are classified by the Drug Enforcement Administration (DEA) into five distinct categories, or schedules, depending upon a drug’s acceptable medical use and potential for misuse. Learn more about DEA drug schedules.
Opioid Dependency Medications
Methadone, buprenorphine, and naltrexone are used to treat opioid dependence and addiction to short-acting opioids such as heroin, morphine, and codeine, as well as semi-synthetic opioids like oxycodone and hydrocodone. People may safely take medications used in MAT for months, years, several years, or even a lifetime. Plans to stop a medication must always be discussed with a doctor.
Methadone
Methadone tricks the brain into thinking it’s still getting the abused drug. In fact, the person is not getting high from it and feels normal, so withdrawal doesn’t occur. Learn more about methadone.
Pregnant or breastfeeding women must inform their treatment provider before taking methadone. It is the only drug used in MAT approved for women who are pregnant or breastfeeding. Learn more about pregnant or breastfeeding women and methadone.
Buprenorphine
Like methadone, buprenorphine suppresses and reduces cravings for the abused drug. It can come in a pill form or sublingual tablet that is placed under the tongue. Learn more about buprenorphine.
Naltrexone
Naltrexone works differently than methadone and buprenorphine in the treatment of opioid dependency. If a person using naltrexone relapses and uses the abused drug, naltrexone blocks the euphoric and sedative effects of the abused drug and prevents feelings of euphoria. Learn more about naltrexone.
Source: https://www.samhsa.gov/medication-assisted-treatment/treatment#medications-used-in-mat
College Depression
“Going to college is an exciting time in the lives of young people, but for some students depression gets in the way. Whether it’s their first brush with the disorder or not, college can act as a catalyst for the onset of depression in many young people, and, on their own for the first time, the timing couldn’t be worse” – childmind.org
Depression in college students is a topic that is not often talked about but is common for first semester college students. Most of the time, first semester students have a hard time adjusting to a new environment; picking up a heavy work load, being away from home, and have to make new friends. Parents can often worry and try to get involved, but that’s not always easy when a child is potentially living three to four hours away from home. If you have a student that is distancing themselves from the outside world, letting go of their hobbies and ambitions, and acting out of character for more than two weeks it is possible that your college student could be facing depression.

Depression is not always an easy topic to discuss, and most people only think an individual is depressed when they are sad. That is not the case, depression comes in many forms. For some students, it could be that he or she is more irritable, lashes out, and pushes away their support systems (friends, family, significant others). Other students could be indulging in binge drinking or substance abuse to try to “forget about their problems” or “make their problems go away”. It is important to notice the signs and act quickly. Encourage your student to seek on campus help or seek help in their area.
If you are worried about your college student and feel that they are facing depression and do not want to acknowledge it themselves, Exult Healthcare has services that can benefit you. Depression is usually treated with medications, psychotherapy, or a combination of the two. If these treatments do not reduce symptoms, transcranial magnetic stimulation (TMS) and other brain stimulation therapies
may be options to explore. However, each case of depression is unique and is treated accordingly. There is never a “one-size-fits-all” for treatments here. Please check out our treatments tab and find out more about how Exult Healthcare can benefit you today.
Written By: Lauren Thompson, Exult Healthcare
BINGE EATING
Binge eating disorder develops based on a mixture of genetic, environmental and social constructs. The focus on this blog is the social/ family aspect of eating patterns.
Food is such a major component of cultural, social and family dynamics. It is used as part of celebrations, for religious ritualization, cultural events and a learned self-soothing habit. We have cake for birthday parties, a cultural dish to help when you are sick (like chicken soup), and a special treat when you are sad (warm cookies) or a special dinner on major occasions. Having food for every occasion can lend to the use of food as a negative coping skill because it has become a learned behavior. Binge eating / obesity will run in families due to the way food is used to deal with feeling or emotions. Memories are strongly tied to our senses: taste reminds use of a positive experience, the smell of food may remind us of a family member that cooked, and touch could be helping cook a special meal and the sound of a specific food cooking to bring back a special memory.
“From infancy, we establish a connection with our caregivers based on how our most instinctual needs are met. “ (Karges, 2018) One of our most instinctual needs is food and it is a major part of the bonding moments with a mother. According to Hamberg, The sharing of food can increases closeness to others like our parents making our favorite dessert when we are upset or sharing food at times of crisis. The use of food can become a supportive behavior and if no other self-soothing behavior is taught then food become the primary means to sooth self and others. The use of food in as a coping and self-soothing tool within the family can lead to binge eating disorders among members. According to Karges, some ways self-soothing through food is taught is by giving a food as a reward, a bribery to behave a certain way or used to comfort a child in destress. It is like replacing their favorite blanket or toy with a cookie every time they get upset.
There is also a genetic connection with binge eating and comorbid disorders like depression so families have learned to cope with the depression by using food. In the study, Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity, There is a correlation between parental mental illness and binge eating disorder and children developing the same patterns of behavior and diagnosis. If the behavior continues then it will be passed down multi-generationally.
The best way to assist in treating or preventing binge eating disorder is through the family system by changing eating patterns and the use of food in emotional regulation. In order for recovery to become effective the family needs to be involved in treatment to help reduce familial patterns in future generations and to support positive change.
References
Braden AL, Madowitz J, Matheson BE, Bergmann K, Crow SJ, Boutelle KN. Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity. Child Obes. 2015;11:1659. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4382825/
Hamburg, M. E., Finkenauer, C., & Schuengel, C. (2014). Food for love: The role of food offering in empathic emotion regulation. Frontiers in Psychology, 5. doi:10.3389/fpsyg.2014.00032 https://www.frontiersin.org/articles/10.3389/fpsyg.2014.00032/full
Karges, K. (2018). Binge Eating Disorder and Family Patterns of Self-Soothing. Eating Disorder Hope. Retrieved from https://www.eatingdisorderhope.com/information/binge-eating-disorder/binge-eating-disorder-and-family-patterns-of-self-soothing.
Written By: Karen Limme LPC Intern, Exult Healthcare

Mainstream Mental Health
Multiple celebrities have opened up about mental health, including the recent news of Demi Lovato’s suspected overdose. In our society, it is easy to idolize those we call celebrities, giving them an image that can be unobtainable.
However, we tend to forget these people are just as human as everyone else.
According to Mental Health America much of our stress can come from everyday responsibilities as well as many obligations and pressures of both physical and mental activities. Celebrities have the whole world looking at them. Imagine trying to eat your breakfast with the twenty strangers taking photos of you trying to catch you spill your orange juice on yourself.
Demi Lovato is not the only one who has opened up about her struggles with mental health. Comedian, Pete Davidson, has also publicly spoken about his battles with sobriety, managing his Borderline Personality Disorder, and troubles with his Crohn’s Disease.
As a mental health facility, we believe awareness of mental health is key. We recently started our free mental health screenings. Allowing anyone to come into our facilities to meet with a mental health professional to learn if they need our services.
The understanding of mental health and all that the illness can ensue needs to be brought to light in our society. Celebrities humanizing themselves by being upfront about their struggles can help those take the needed steps to join the conversation to receive the help they deserve.
Written by: Kimmie Thompson, Exult Healthcare

Perpetuating the Negative
Most of us have maladaptive thinking habits that lead us into anxiety, depression or substance use. It’s based on our environment and how we learned to think based on the family, social, economic, ethic, religious and political background that we grew up within. We get stuck in the unhealthy thinking habits and we get stuck in a loop.
- What drives the old habits of thinking:
- Living on automatic pilot instead of awareness and conscious choice
- Relating to experiences through thought rather than direct sensing
- Dwelling on and in the past and future rather than being fully in the present moment
- Trying to avoid, escape, or get rid of unpleasant experiences rather than approach it with interest
- Needing things to be different from how they are rather than allowing them to just be as they already are.
- Seeing thoughts as true and real rather than as mental events that may or may not correspond to reality.
- Treating oneself harshly and unkindly rather than taking care of oneself with kindness and compassion.
(Segal, Williams & Teasdale, 2013, p. 89)
Keeping these thinking habits can lead to worse habit forming behaviors. It becomes a coping mechanism for some and a way to stop progressing for others. Whenever you are struck into a loop of negative thinking, positive can change things around. Although thinking positively is easier said than done. Minor adjustments can help break a negative cycle such as:
- Change and observe your body language
 Talk it out
Talk it out- Take a walk
- Spend one minute of meditation
- Have a cup of tea
- Positive affitmations
By LPC-Intern, Karen Limme
Quotes on Thoughts:
“Thoughts are not facts.”
(Segal, Williams & Teasdale, 2013, p. 164)
“A thought is a mental event containing a seed of reality surrounded by a shell of inference”
(Segal, Williams & Teasdale, 2013, p. 313)
“If we can observe in ourselves the toxicity of certain beliefs, thought patterns, and behaviors as they arise in the moment, then we can work to lessen their hold on us.”
(Kabat-Zinn, 1990, p. 217)
Reference:
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness (15th anniversary ed.): New York: Delta Trade Paperback/Bantam Dell.
Segal, Z., Williams, M., & Teasdale, J. (2013) Mindfulness-based cognitive therapy for depression. New York: Guilford Press.

